The use of antiepileptic drugs in the prevention of clozapine-induced seizures. Literature review
Wioletta Żukowicz, Wiesław Jerzy Cubała
 Affiliacja i adres do korespondencji
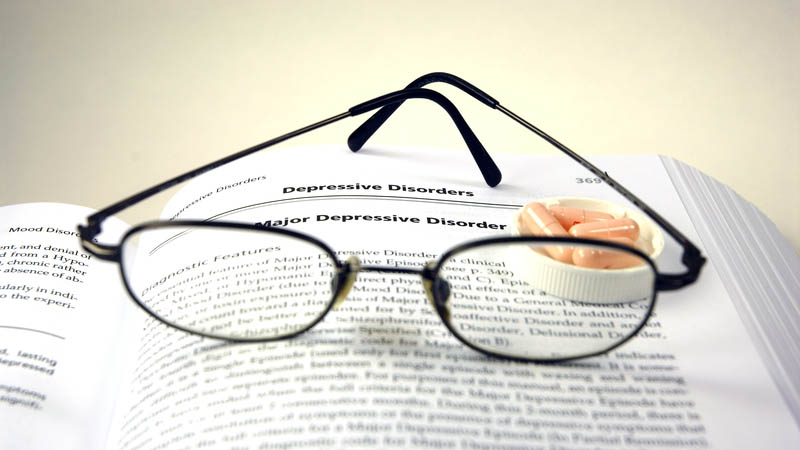
Affiliacja i adres do korespondencjiClozapine is an atypical antipsychotic used in the treatment of drug-resistant schizophrenia. Due to its safety profile and the risk of severe adverse effects clozapine is not a first-choice medication. The most crucial adverse effects include bone marrow suppression leading to agranulocytosis (defined as neutrophil level drops below 500/mm3) and cardiomyositis. An increased risk of orthostatic hypotonia, bradycardia, syncope or cardiac arrest has been observed during therapy. Therefore, it is recommended that clozapine should be used with caution in high-risk patient populations, particularly in patients with cardiovascular disorders and cerebrovascular diseases, as well as those predisposed to hypotension (dehydrated patients, patients receiving hypotensive agents). Serious adverse effects further include an increased risk of seizures. Among all antipsychotic drugs clozapine has the greatest potential to decrease the threshold for seizures. The risk of seizures is particularly high when clozapine is administered at a daily dose of ≥600 mg and in the case of rapid dose increases. Caution should be exercised when treating patients with additional seizure risk factors, such as central nervous system disorders, medical history of epilepsy, alcoholism or receiving medications that decrease the threshold for seizures. So far, no clear guidelines have been set indicating the necessity of a simultaneous use of antiepileptic drugs to prevent clozapine-induced seizures. This paper reviewed the literature on the influence of various factors on clozapine serum levels, risk assessment of seizures in the therapeutic process as well as the use of antiepileptic drugs in seizure prevention.