Application of neuropsychological assessment in a patient with posthaemorrhagic hydrocephalus – a case report
Agnieszka Pawełczyk, Jakub Jankowski, Ryszard Twarkowski, Klaudia Korona, Weronika Lusa, Maciej Błaszczyk, Maciej Wojdyn, Maciej Radek
 Affiliacja i adres do korespondencji
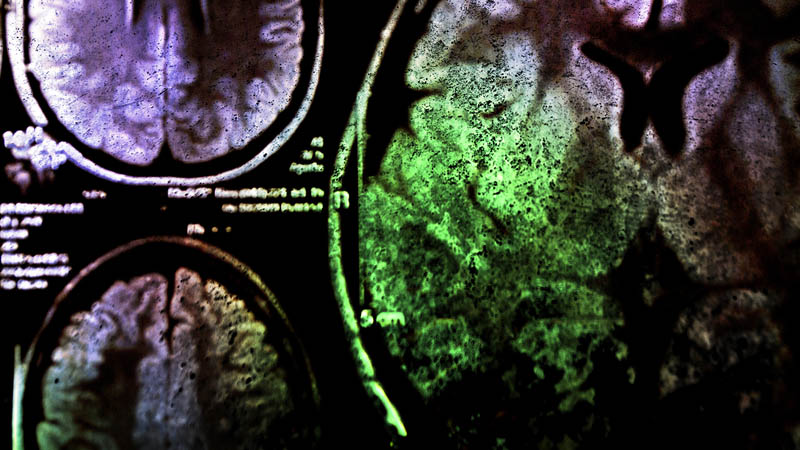
Affiliacja i adres do korespondencjiIntroduction and objective: Posthaemorrhagic hydrocephalus constitutes one of the most serious complications of subarachnoid haemorrhage. The most common cause of subarachnoid haemorrhage is a ruptured intracranial aneurysm. Clinical and neuropsychological presentations of the posthaemorrhagic hydrocephalus include mainly gait apraxia, urinary incontinence, and various neurocognitive impairments. The main neurosurgical treatment of the posthaemorrhagic hydrocephalus is ventriculoperitoneal shunt implantation. The study aimed to analyse the neuropsychological functioning of a patient with post-haemorrhagic hydrocephalus, describe the dynamics of cognitive changes during hydrocephalus, and emphasise the importance of neuropsychological diagnosis in planning neurosurgical intervention. Materials and methods: In this article, we report a case of a 52-year-old male patient, who suffered from subarachnoid haemorrhage after an anterior communicating artery complex aneurysm rupture. After the surgery, the patient presented with massive episodic memory deficits, periodical illogicality, and disorientation. Neuropsychological examination, conducted using Addenbrooke’s Cognitive Examination III (ACE-III) in parallel versions and the Trail Making Test A and B (TMT-A and TMT-B), showed deterioration of psychomotor speed, decreased concentration of attention and impaired executive functions. Results: Due to the gradual neurological condition improvement, the patient was discharged from the hospital but four months after the surgery, he was readmitted with gait apraxia, a decline in cognitive and executive functions in neuropsychological examination, and radiological signs of hydrocephalus in the computed tomography. The patient underwent a ventriculoperitoneal shunt implantation, but due to the suspicion of iatrogenic peritonitis, the ventriculoperitoneal shunt system was removed. The recurrence of the clinical and neuropsychological symptoms was observed and ventriculoperitoneal shunt reimplantation was necessary. The surgery was performed after seven weeks. In the postoperative course and followup examination, the patient was again in logical contact, did not show any cognitive decline and did not present any clinical disturbances. Conclusions: Thus, we demonstrated the importance of neuropsychological assessment in the diagnosis of posthaemorrhagic hydrocephalus and the clinical and psychological characteristics of the patient with shunt-dependent hydrocephalus with the presence of neuropsychiatric symptoms. This study shows that neuropsychological examination is highly sensitive to detection of subtle changes in the cognitive and emotional functioning of a patient with hydrocephalus, which are early signs of deterioration of the patient’s neurological condition and changes in the ventricular system.